A key issue in the diagnosis of mTBI is the identification of clinical markers that may be used to ensure an accurate diagnosis of the injury. The classical diagnostic tool remains the Glasgow Coma Scale (GCS). It is however, known that it is possible for an individual to suffer neurological insult and remain asymptomatic. It is also known that it is possible for an individual to suffer neurological insult and remain unaware of the injury due to a lack of knowledge of brain trauma, of its manifest symptoms, a misinterpretation of the associated signs and symptoms, or due to cognitive masking associated with the injury itself.
The situation is compounded by the fact that mTBI injury may not be seen on standard forms of diagnostic imaging such as CT, or MRI T1, and T2, scans. Neuropsychological testing has demonstrated the ability to identify cognitive deficits equivalent to a 10% loss of prior cognitive function when testing is conducted in close association with a prior baseline test. If no recent baseline test is available, then such a minor loss of cognitive function is unlikely to be recognized in a clinical diagnostic setting. Neuropsychological testing is expensive, with the cost of single test suite ranging from $2,000 to $4,000 dollars, a cost normally not covered by public health insurance. Advances have been made in the search for serum bio-markers of mTBI, but no reliable clinical test is presently available. Even if such bio-markers were found to have clinical validity, there is the issue of the unsuspecting victim failing to present themselves for diagnosis for the reasons set out supra.
This post introduces a potential diagnostic technique, one which may have broad application both in clinical settings, and for the purpose of initial field screening for injury.
In the Feasibility of the Neurological Outcome Scale for Traumatic Brain Injury (NOS-TBI) in Adults, Wilde et al. 2010, examine the use of a scale intended to be employed in a clinical setting for the diagnosis of all severity of TBI injury: “The NOS-TBI may serve a role in clinical practice in patients with TBI similar to the way the NIHSS has functioned for patients following stroke, by serving as a tool for initial stratification of injury severity, and as an outcome measure in clinical trials.”
The content validity of the NOS-TBI “was established by a panel of recognized experts from a wide range of relevant backgrounds (drawn from two Level 1 trauma centers in a large metropolitan area) who regularly treat patients with TBI at varying points in recovery, including two neurologists, a neurointensivist, a physiatrist specializing in TBI rehabilitation, two neurosurgeons, and four neuropsychologists specializing in TBI.” The background to the instrument, and the process of instrument development is described in the paper available here.
Wilde et al. (2010), made a number of modifications to an existing instrument, the National Institutes of Health Stroke Scale (NIHSS), which has experienced widespread adoption for the identification of neurological deficits associated with stroke. One modification of specific interest addresses hearing loss and reflects the high incidence of hearing loss in TBI victims: “The incidence of sensorineural hearing loss associated with nerve injury (CN VIII) has been reported to be as high as 85% in TBI (Podoshin and Fradis, 1975)”.
The author is currently engaged in litigation with an insurer who has denied his claim. One ground for denial is the lack of objective supporting evidence of injury. Standard MRI testing gave no evidence of neurological insult. At the behest of his treating doctor, the author underwent a hearing test in 2014 but he completely forgot about this test until a retest opportunity became available. Review of the 2016 retest demonstrated a hearing loss profile identical to that found in the original 2014 test. These findings are reviewed in this January 12th, 2016 post.
The author conducted additional research to gain a better understanding of the clinical implications of the evidence obtained from the test/retest sequence. This brought the above Wilde et al. (2010), paper to his attention, especially the statement that 85% of TBI victims suffer from “sensorineural hearing loss associated with nerve injury`.”
A second research paper was found that provides supporting evidence. Entitled Hearing Loss and Vertigo Secondary to Head Injury it was published in The New England Journal of Medicine 1982; 306:1029-1031, April 29, 1982: DOI: 10.1056/NEJM198204293061705. The author lacks the funds to access the entire article. In lieu of an abstract, the first 100 words are presented on The New England Journal of Medicine website here. This 100 word text is as follows:
“VEHICULAR accidents represent the single greatest cause of death and injury to people under the age of 35 in the United States. Approximately 75 per cent of these accidents involve injuries to the head. Cochlear and vestibular dysfunction represent the largest group of delayed complications of head injury that can be objectively demonstrated. Historically, vestibular and cochlear dysfunction after such injuries was considered irreparable, and therefore otologists were seldom consulted in such cases. In 1956, objective evidence was presented to demonstrate that ossicular-chain injury and subsequent conductive hearing loss could follow head injury. This represented the first evidence of a .” (Emphasis added in bold)
Further confirming evidence was obtained from a study found in the Indian Journal of Otolaryngology and Head & Neck Surgery, 2011 Jan; 63(1): 45–49; doi: 10.1007/s12070-011-0117-x (Full text here). The abstract provided a succinct overview:
“Hearing loss is a common problem encountered in ENT practice. Hearing loss following head injury is a major medical problem in both adults and children, which may go unnoticed when it does not affect speech frequencies. Sensorineural hearing loss at high frequencies is a common finding in minor head injury.”
The paper describes the outcomes of a study of 60 traffic accident victims with GCS of 13-15, age between 6 and 60 years, and LOC of less than 20 minutes. “A total of 62% had hearing loss, the most common frequencies affected were 4000 and 8000 Hz (Fig. 3).”
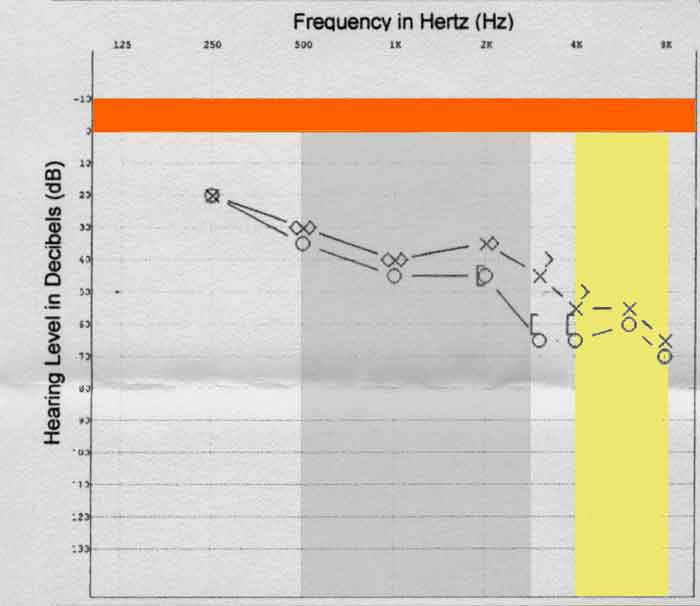
Figure 1 – January, 2016 Hearing Test Result
Figure 1 shows the author’s 2016 test result. All entries below the horizontal orange bar represent hearing loss. The rectangle shaded in yellow represents the range of frequencies between 4000 and 8000 Hz, the frequencies most commonly affected by TBI injury.
A paper in the Journal of the Korean Neurosurgical Society, Detection of Traumatic Cerebral Microbleeds by Susceptibility-Weighted Image of MRI (J Korean Neurosurg Soc. 2009 Oct; 46(4): 365–369; doi: 10.3340/jkns.2009.46.4.365) available online here, describes a study concerning 21 mTBI patients without any parenchymal hemorrhage on conventional MRI, and a 42 person control group with no brain trauma, who were tested for the presence of cerebral microbleeds (MBLs) using Susceptibility-weighted image (SWI) MRI.
Figure 1 in this October 2009 article presents evidence of a 50 year old man who complained of left side hearing difficulty after head trauma. Investigation of this injury by MRI gave no evidence of hemorrhagic injury. The original figure is reproduced below:
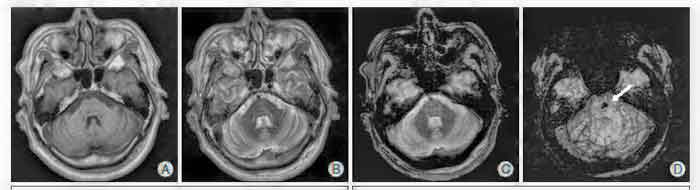
Figure 2 – Comparison of MRI and SWI imagery in Detection of Microbleeds
MRI images A, B, and C, show no evidence of MBLs. SWI image D does show a microbleed (White arrow points to the area of the microbleed). The same individual was tested for hearing loss. The result of this testing is shown in Figure 3 below.
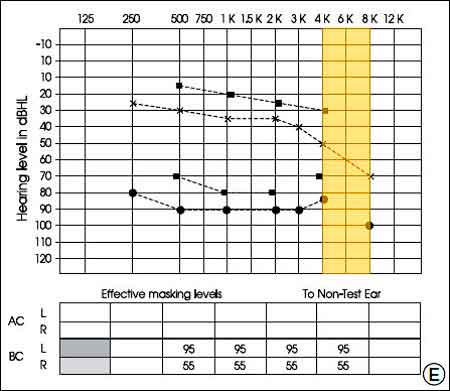
Figure 3 – Hearing Test Results From 50 year old with Head Trauma
The decline in hearing in the frequency range from 4000 to 8000 Hz is evident.
Discussion of mTBI Diagnostics – Hearing
Given that hearing loss may be prevalent in a significant majority of head injury victims, it is suggested that persons presenting with head injury be given a hearing test. Since the victim is likely to be unaware of hearing loss post-injury, the test should be applied as part of the normal investigation of a possible mTBI.
The fact of high frequency hearing loss as a marker of mTBI also suggests an opportunity to provide an accessible means of early identification of mTBI injury. Since “ìt is important to identify and treat TBI victims as early as possible,” [Int J Mol Sci. 2015 Jun; 16(6): 11903–11965; doi: 10.3390/ijms160611903], consideration should be given to the creation of a test instrument that may be easily and quickly deployed at the site of the injury. This is especially true given that many victims of mTBI may remain unaware of their injury, or may fail to recognize, or may misattribute, the available signs of injury.
The majority of the population presently carries a cell phone. Most of these devices also double as portable music players and this alternate use is a key selling point, especially among the younger population who are at greatest risk for mTBI injury. High quality sound reproduction is therefore an engineering and marketing requirement.
It should be possible to devise an application that delivers a series of pure tone signals in a range of frequencies and obtain user feedback in regard to the recognition of those frequencies. Individuals who demonstrate a loss of higher frequency hearing may then be directed to seek medical attention.
The validity of this test would likely be improved if the application offered an initial pre-test sequence at the time of user registration. When the user first opens the application, they may be provided with explanatory text on the intended use. They may next be guided through the conduct of an initial baseline test which is either stored within the application. or transmitted to an online repository.
At the time of a suspected injury, the individual conducts a retest and the retest data is compared with the stored baseline data. If there is significant variance between the two test results, the user may be cautioned in regard to the possibility of having sustained an mTBI and be directed to seek appropriate medical attention. (There are a number of ways by which the utility of this application may be enhanced. These are not described here.)
There is a secondary benefit to having such an application available. It is well understood that exposure to loud sound over a period of time may result in hearing loss. The same test instrument may offer the benefit of providing a means of assessing this loss due to noise exposure. These tests offer a means to empower the individual and guide them to exert greater control over their own health while appraising them of the negative outcomes associated with disregard for their health. There exists the potential to introduce a heightened sense of personal responsibility for individual well-being, coupled with the means to identify a potential negative health variance. This set of outcomes may be of considerable interest to public health authorities who would find it to be in the public interest to fund the associated research and development activity as a long term cost reduction measure.
Since the proposed application would receive strong parental endorsement, it is highly likely it would find its way to being installed on those cell phones parents provide to their offspring. A significant branding opportunity is therefore available and this may represent an alternate source of development income and / or provide a long term revenue stream which may be directed to further research into mTBI and similar programs ((See the Proposal: TBI Rehabilitation available here).
It is noted that if the application is designed to upload baseline data to a repository, then it will be possible to use the collected data to perform significant research on the numbers of individuals at risk, the nature of the hazards to which they are exposed, the injury incident rate per 1,000 population, the nature of the injury sustained, the treatment delivered, and injury outcomes. It is recognized that much mTBI injury goes unreported due to the imperfect knowledge of both the public and treating professionals. The introduction of an application as described here would serve to correct such deficiencies.
